UNOS runs the national Organ Procurement and Transplantation Network (OPTN). The OPTN coordinates over 400 medical entities to provide the equitable allocation of organs and appropriate professional standards for life-saving transplants throughout the United States. The ethics issues involved in making this daily equitable allocation are sensitive and newsworthy.
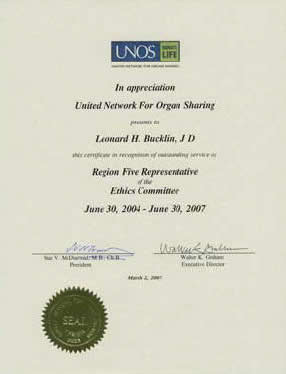
Bucklin served on the Ethics Committee of UNOS for a dozen years.
- Through a national Organ Center, UNOS matches donors to recipients 24 hours a day, 365 days a year.
- UNOS develops the national regulations and policies that maximize the limited supply of organs and give all patients a fair chance at receiving the organ they need — regardless of age, sex, race, lifestyle, financial or social status.
- UNOS sets professional standards for ethical, efficient and quality patient care in transplant hospitals.
- Through the Organ Center, UNOS manages the national transplant waiting list.
- UNOS maintains the database that contains all clinical transplant data. These data are used to improve the medicine and science of transplantation, develop organ allocation policy, aid scientific research and support transplant professionals in caring for patients.
- UNOS monitors every organ match to ensure adherence to UNOS policy.
- Through nationwide publicity campaigns, UNOS raises public awareness about the importance of organ donation.
Ethics, law, and medicine are all involved in this corporation’s setting of national priorities, hospital and medical regulations and policies. UNOS is the federal contractor running the Congressional mandated national Organ Procurement Transplant Network, (OPTN). UNOS and the OPTN must balance a multitude of factors and competing interests of the average 85,000 persons awaiting life-saving organs every day (when only about 25,000 organs are available during a year).
Every day the OPTN operations center makes individual allocations and arrangements for securing tens of thousands of organs, transporting them, and providing to which transplant center and patient to whom they are allocated. The OPTN mandates standards for organ transplantation professionals and hospitals and audits for the Government the performance of the over 400 organizations across the country involved in transplantation.

Woe Unto Those Who Request Consent: Ethical and Legal Considerations in Rejecting a Deceased’s Anatomical Gift Because There is no Consent by the Survivors
Leonard H. Bucklin
North Dakota Law Review, Vol. 78, October 2002, Copyright
Abstract:
The thesis of this article is that it is unethical (and legally dangerous) for an Organ Procurement Organization (OPO) to refuse a decedent’s gift of organs on the basis that a next of kin does not give consent to the OPO’s receipt of the gift.
Statistics may indicate that we do not have a shortage of organs for transplants; we only have a shortage of organs recovered. Certainly part of the organ shortage is caused by the practice of Organ Procurement Organizations (OPOs) to refuse a decedent’s gift of organs on the basis that a next of kin has not given consent to the OPO’s receipt of the gift. The legal and legislative communities have for years tried to convince the OPO’s to accept the gifts without seeking consent of the survivors. The Uniform Anatomical Gift Acts of 1968 and 1987 were such attempts by the legal and legislative communities. Although the practice is changing, many OPOs continue in the practice of requiring “consent” by survivors to a valid anatomical gift made by the deceased.
The author proceeds on the assumption that an extensive discussion of the legal issues, coupled with a discussion of the ethical issues, may change practices of OPOs and thereby increase the rate of organ recovery.
Part one of the article examines the legal rights of the deceased, the OPO, and the survivors in a dead body. The history of the law of dead bodies and the Uniform Anatomical Gift Act, adopted in some form in every state of the United States are reviewed. Then the legal liability issues in obtaining cadaveric organs for transplantation when the next of kin objects, or is not present to give consent, are discussed. The legal theory indicates there is no liability to accepting a valid anatomical gift without further “consent”, and indeed the reported legal cases unanimously support non-liability for following the Uniform Act, regardless of the objections of the next of kin. On the other hand, denial of the gift only to seek “consent” from others may impose liability on the OPO, and these possibilities are laid out for future litigators.
Part two of the article analyzes the ethical principles involved when an OPO requests consent when it is known (or should be known if a reasonable search was made) that the deceased had signed an organ donor card. The ethical principles of utility, justice, and autonomy all are violated by OPOs that seek unnecessary consent. Such OPOs violate the ethical rights not only of the deceased, but also of the patients waiting transplant.
The article concludes that there is no legal reason not to accept the gift of the decedent; and that the OPO has an ethical duty to accept the gift of the decedent. It is unethical (and legally dangerous) for an OPO to refuse a decedent’s gift of organs on the basis that a next of kin does not give consent to the OPO’s receipt of the gift.
Keywords: organ transplantation, Uniform Anatomical Gift Act, Organ Procurement Organization, consent, ethics
JEL Classifications: I18, I19, K11, K32